Displaying items by tag: ultrasound
The LOVE Approach Ultrasound Clinical
REGISTRATION IS NOW OPEN!
Join us in Cincinnati, Ohio,
on March 25-27, 2026
Subscribe here to receive the latest information on clinicals and registrations.
"This fits exactly how I want to practice medicine.
It’s evidence-based and rigorous.
It has integrity and incorporates God.
Medicine is fast, just like this week.
This is how medicine should be practiced."
- LAUC Attendee, July 2024
"[Our Medical Director] absolutely LOVED it!!!
She learned so much and she has recommended that
our future medical team will attend this training for ultrasound.
She said it was comprehensive and LOVED the
spiritual component to the training, which
provides life-long networking.
Thank you so much for all you do! "
- LAUC Attendee, Fall 2025
While there are various ultrasound trainings available for nurses and sonographers who work within the pregnancy help movement, Heartbeat International has championed a new form of training that connects the technical needs and the spiritual needs for those working in pregnancy help. The training is held in two parts: First, students complete an online ultrasound training* through Heartbeat International’s Academy, which meets the Association of Women's Health Obstetric and Neonatal Nurses (AWHONN) guidelines for didactic training, as well as completing 25 abdominal and 5-10 transvaginal limited obstetrical scans as a prerequisite** to prepare for the in-person training. Next, students come on-site to participate in an in-person scan lab experience with one-on-one instruction from educators who are also sonographers credentialed in RDMS (OB/GYN) and RNs who have multiple years of experience imaging in Pregnancy Help Clinics.
By combining the technical, practical, and spiritual elements into one pregnancy help medical training, trainees will work towards becoming equipped, qualified, and ready to scan within their center. (Looking for training for other Pregnancy Help staff? Click here!)
This Clinical will include:
- 50+ Scanning Drills
- Pregnant models of all gestations
- Unique L.O.V.E. Approach Method of imaging the preborn babies
- Competency scanning pathology is typically encountered in Limited Obstetric Diagnostic Ultrasound
- First simulation training offered nationally in the Pregnancy Help movement
- Transvaginal instruction on simulation models
- Mastering skills by scanning a simulated ectopic pregnancy
- Image Reviews
- Spiritually focused instructional approach
- Case Studies
- How to introduce a mom to her baby for the very first time
- Skills Evaluations for those completing training
- Supportive team to reinforce your calling
*Heartbeat International will offer 20 Continuing Education Contact Hours for nurses for the didactic portion of training and 12 Continuing Education Contact Hours for nurses for the clinical portion of training. Heartbeat International is an approved provider through the California Board of Nursing, Provider Number 16061.
The focus of the clinical event is on repetition and volume, along with spiritual encouragement and reinforcement of techniques and knowledge gained from the didactic training. The ideal participant is someone who is self-motivated and confident and needs a high volume of scans for training. This event is fast-paced and filled with drills, techniques, and one-on-one instruction from educators who are also sonographers credentialed in RDMS (OB/GYN) and RNs who have multiple years of experience imaging in Pregnancy Help Clinics. Each participant receives a skill evaluation by our instructors; however, Heartbeat
Are you concerned about retaining nursing staff after investing in ultrasound training? We understand this may be a concern. That’s why we’ve gathered data from our LAUC training events to help put your mind at ease—and show you the lasting impact of this investment:
- Post-event surveys show that 98% of those who attended LAUC continue to work in pregnancy help
- After one year, 93% of attendees have continued in their clinic roles
NEW! Take a look inside The L.O.V.E. Approach Clinical by listening to Lisa Bourne and Christa Brown discuss how The L.O.V.E. Approach can be effectively used in the ultrasound setting, and how attending the Clinical not only gives you technical experience but also teaches students to deal with the spiritual warfare that we see on the pro-life battlefield. Click here ![]()
Pricing
The L.O.V.E. Approach Ultrasound Clinical includes 20 hours of didactic training (20 CEUs) and 24 hours of clinical training (12 CEUs).
| Affiliates | Non-Affiliates | ||
| Early-Bird | $1,950 | $2,200 | Until 2/14/2026 |
| Regular | $2,200 | $2,450 | Until 3/7/2026 |
- You must complete the didactic portion of Heartbeat's Online Ultrasound Training. You will not be permitted to scan without having met this requirement. You should be automatically enrolled in the didactic training within one business day and will receive an email to complete the training at www.HeartbeatAcademy.org. If the registered attendee has not received an email from Heartbeat International within 36 business hours of the registration, please let us know immediately.
- In order to get the most out of your time with us, you must complete 25 abdominal and 5-10 transvaginal limited obstetrical scans before arriving at the training site.
**Nurses attending the LOVE Approach Ultrasound Clinical have found many ways to obtain the prerequisite of 25 abdominal and 5-10 transvaginal limited obstetrical scans. Here are a few ways to fulfill this requirement.
- Scan with another clinic. Here is a locator to find nearby pregnancy help organizations.
- Offer a scanning day to scan clients who have been scanned previously with a sonographer or a trained nurse.
- Scan some women who are not pregnant (such as coworkers or friends) to image female anatomy and to become acquainted with the function of an ultrasound system.
- Contact a local OB office for possible assistance with training scans.
Hotel & Other Helpful Information
*Please remember your registration does not include your hotel accommodations.
A booking link or recommended lodging will be included in your registration confirmation email.
The training will take place at Embassy Suites by Hilton Columbus Dublin. Please use the room block booking link in your registration confirmation email to receive a special room rate.
We recommend that you wait to book airline reservations until your LAUC registration has been confirmed, as these trainings tend to fill up quickly.
Training Schedule
-
Tuesday: Travel day. Check-in at the hotel is available starting at 4:00 p.m. Early check-in may be available if rooms are available.
-
Wednesday-Friday: will include all-day sessions (typically 9 a.m. to 5:00 p.m.). We will end at 4:00 p.m. on Friday to allow travel home.
Meals
Lunch meals will be hosted at the training facility.
Attention Affiliates: Be sure to log in as an affiliate using the button in the top right corner of the webpage to receive a discount on the pricing below. (Go to “My Affiliate Dashboard” to make sure your organization is listed. If it is not listed, reach out to awood@heartbeatinternational.
Mark your calendars for these future dates!
Watch Highlights From Our Last Event in Colorado!
Exciting News about Heartbeat's Online Ultrasound Training!

Our completely updated training will be available in early March for medical professionals offering Limited Obstetric Diagnostic Ultrasound in Pregnancy Help Clinics. We are thrilled to offer ten new modules on topics such as ultrasound physics, first trimester scanning, legal and ethical questions, knobology, and more.
We invite imagers around the world that perform limited obstetric diagnostic ultrasounds to our updated Online Ultrasound Training. The purpose of scanning in the Pregnancy Help Clinics is to shed His Light on the reality of life by showing a mom the first image of her baby. Designed with the medical professional in Pregnancy Help Clinics in mind, this training is rooted in the LOVE Approach for all who serve and all who are served in Pregnancy Help Clinics.
Available to you:
- Preparation for the imager for the front lines
- Image review by sonographer trainers for one full year
- Community calls with sonographer trainers and other students
- Handouts for all training modules
- Self-paced training for the busy nurse
- Video training and demonstration
- Clinical component completed in your own center
- Access to the didactic training for six full months
- Nursing and ARDMS CEUs
(SDMS does not require continuing education credits)
Training topics includes:
- Legal and Ethical issues of Limited Obstetric Diagnostic Ultrasound
- Nursing Professional Practice Guidelines
- Patient Assessment and Education
- Ultrasound Instrumentation & Imaging Techniques
- Typical and Atypical Findings
- Doppler and the Fetal Heart
- Policies, Procedures, and Protocol
- Ultrasound and the Abortion Pill Reversal Client
- Obstetrics and Prenatal Health
- Ergodynamics
- The Physics of Ultrasound
- Fetal biometry in Limited Obstetric Ultrasound
- And more!
Who are the instructors of this course?
You will not walk the journey alone but rather will be guided by those of us who have walked the journey before you. Each member of the Medical Impact team has been a part of creating this training and providing support for you as you learn.
Gathered from around the world, we are dedicated to assisting and encouraging while you learn not only the technique of performing a Limited Obstetric Ultrasound Diagnostic Exam but also as you forge through the spiritual warfare that will accompany it.
Our team is composed of sonographers that are multicredentialed to include RDMS(OB/GYN) and recognized nationally for their accomplishments and Registered Nurses that have performed ultrasounds in Pregnancy Help Clinics throughout the nation. You will also hear from Heartbeat International General Counsel, HBI President Jor-El Godsey, Vice-President of Ministry Services Betty McDowell, and Vice-President of Development Cindi Boston-Bilotta and others from the HBI team. Each member of this team brings with them experiences that will enhance your learning experience.
Who is this course designed for?
This course was created for medical professionals who are called to perform ultrasound in Pregnancy Help Clinics. It is not essential for you to obtain the RDMS credential to effectively perform Limited Obstetric Diagnostic Ultrasound. It is essential that you become competent. This course is designed with you in mind. We fully believe that God equips who He calls!
What is the pace of the course?
This training is self-paced and can fit in any schedule. Participants complete modules when convenient to their them. There are no required log-in times but we would expect the course to completed within six months from start date. Recognizing that each person will progress at his or her own time frame, the clinical section of this course can be completed while one is completing the didactic portion of the program or may be completed following the completion of the program.
What topics are included?
Module I The Power of Seeing
This module explores a basic overview of the history of Ultrasound and its unique utilization in Pregnancy Care Centers.
Module II: Limited Obstetrical Ultrasound for the Registered Nurse
These presentations provide guidance on patient assessment & education, documentation, and nursing professional practical guidelines for those that scan in Pregnancy Help Clinics.
Module III: The Physics of Ultrasound
These presentations will help you become more familiar with you machine along with teaching basic physics principles that will enhance your scanning effectiveness.
Module IV: Pelvic and Obstetrical Anatomy
This module will briefly review basic embryology along with the female reproductive system and basic first trimeter obstetrical anatomy in order to prepare the participant for First Trimester Obstetrical Ultrasound.
Module V: Obstetrical Ultrasound
These presentations focus on the basics of scanning in the first trimester starting from basic transducer manipulation to basic measurements along with presentation techniques.
Module VI: Normal Variants and Atypical Findings
These presentations focus on scanning beyond the typical first trimester scan concentrating on the second and third trimester basic measurements, presentation techniques, commonly encountered first trimester abnormalities and scanning multiple gestations.
Module VII: Abortion Pill Reversal and Ultrasound
These presentations will help you to care for the abortion pill reversal client in your clinic.
Module VIII: Legal and Ethical Issues
This module concentrates on quality analysis of exams along with legal and ethical issues.
Module IX: Self-Care and the Imager
This presentation explores the personal role of the imager and the care that is involved in those who serve on the front lines.
Module X: Clinical Competencies
The clinical component of your training includes two elements, an experience log and competency evaluation. Clinical portion of training is completed in your clinic under the supervision of a qualified RDMS OB/GYN Sonographer, qualified RN who has completed ultrasound training, or a Physician of your choice.
What is included in these modules?
Each module of this course consists of presentations, discussion questions, and assignments. This course is designed to be completed in its entirety with each section developed to specifically prepare students for the task ahead. After each section, a small quiz assesses understanding of the topic. Questions are encouraged in the discussion forum or in email to our ultrasound instructors.
What is the cost?
Cost is $495 for non-affiliates/$395 with HBI affiliate discount.
Assistance is available to centers who qualify through the Option Ultrasound Program (OUP) which provides grants to qualifying pregnancy medical clinics for 80% of the cost of an ultrasound machine or sonography training for medical personnel.
We are excited for those that will join us on this endeavor to image life. We can assure you, this will be a life changing experiencing for you and those for who you scan!
For more information:
Contact our Medical Impact Team at This email address is being protected from spambots. You need JavaScript enabled to view it.
We are thankful to all that heed the call of obedience and using your medical background for the unborn child.
Provider approved by the California Board of Registered Nursing, Provider Number CEP 16061 for eight contact hours.
Dear Board Member . . .
At the end of Pregnancy Help Institute, we invite our attendees to write a letter to the Board of a pregnancy center who might be trying to decide whether to send staff for training or not. Every year, we are inspired by their reactions to working with other like-minded individuals as they sharpen their skills to continue serving on the front lines of pregnancy help. Here's what a few of our 2017 Pregnancy Help Institute graduates had to say.
Dear Board Member,
If you are looking for one single thing that you can do to grow the ministry that you are a part of, please consider sending your director to Pregnancy Help Institute. I know when the budget is tight it is hard to spend money and allow your director to be out of the office. But it is worth every penny. Equipping your director to do his/her job better is a huge part of Pregnancy Help Institute, but the encouragement they will find there, you cannot put a price tag on.
Sincerely,
2017 Pregnancy Help Institute Graduate
New Director Track
Dear Board Member,
If you are considering sending your medical staff for ultrasound training at Pregnancy Help Institute, please do it! It will equip your staff to not only learn/be able to perform basic ultrasound exams, but to give that mother a chance to view LIFE! Not only will they learn the skill of ultrasound, but they will also be encouraged spiritually to effectively help a mother see her unborn. Your staff will leave blessed when they go in, and blessed when they leave (Deuteronomy 28:6).
Sincerely,
2017 Pregnancy Help Institute Graduate
Ultrasound Training Track
Dear Board Member,
What I have discovered is how important it is to take some time away to refresh and rediscover our purpose and energize our soul for the work we do. Being a part of the Pregnancy Help Institute training in development has helped me not only affirm much of what I have been focused on, but also to discover new ways to take our ministry to the next level. Development involves everyone on the team, and I have taken away so many ideas that I can present to our team to help us be the best we can be.
This week, I have been challenged, affirmed, and inspired to take what we do for God to the next level. I can take my skill set and use it for so much good. I have met amazing people who I will keep in touch with and bounce new ideas off of. It is so important to value the resources we have through Heartbeat International and to allow your team to participate so that they are more equipped to serve women and their families and affect generations to come and most importantly, be able to put on the armor of God to do the work we have been called to do. It’s an investment for God.
Sincerely,
2017 Pregnancy Help Institute Graduate
Development Track
Dear Board Member,
The investment for the heartbeat International training is not only faith-filled, but full of amazing information that can and will be incorporated into our plans for the home. I firmly believe this is something new members, as we add them to our team, need to attend. Not only has it been an amazing and information-filled week, but it has renewed my fire and excitement for our ministry.
Thank you,
2017 Pregnancy Help Institute Graduate
Leadership Track
2017 Ultrasound Training at Pregnancy Help Institute a Huge Success
The 2017 Pregnancy Help Institute Ultrasound Track was a great success!
Heartbeat International was incredibly blessed to have Tammy Stearns, RDMS and Bryan Williams, RDMS facilitate the ultrasound training portion of PHI. Tammy and Bryan, along with several other volunteer sonographers, spent the week training ten participants, including nurses, an RDMS, a Nurse Practitioner and a physician, from Pregnancy Centers around the country. Trisonics and Preferred Medical Systems, in a joint collaboration, provided ultrasound machines for use during the week of training.
The ultrasound training not only contained a didactic portion and scan labs, but a spiritual component as well. Tammy opened each day reminding the class that this is a ministry, not just a skill, and that this ministry is something that can only come out of God’s overflowing presence in our lives, and not from within our own selves. Each day, Tammy’s devotions emphasized how the spiritual side of things was a big part of the ultrasound ministry.
“I appreciate that this training was tailored to working in a CPC. I learned not only technical training but the spiritual aspect of giving these babies a voice for the first time.”
Each morning there was a classroom-style teaching which covered topics from physics and QA in the ultrasound setting, to anatomy of mom and baby, and abnormal findings while performing ultrasounds. For many of the participants, this was the first time they had undergone such a training, and the curriculum was designed to be real and applicable.
The afternoon scan labs were a huge success. There were 7 instructors who were involved in the hands-on training, and about 40 “models” from the community who volunteered their time (and bellies) for the students to take turns scanning. In total, about 200 scans were performed by the class (about 20 per student) which went towards the recommended 50-75 training scans that is recommended for Limited OB Ultrasound training. The students learned the basics of scanning a typical client that may present in the PRC, as well as the unique instruction on how to dialogue with the abortion-minded client during a scan.
“This was a very informative training. Each sonographer had a helpful hint to give, each one gave critical information for getting good ultrasounds. The didactic information was explained fully and in a helpful way. I believe I got way more than my money’s worth.”
The overall success of this year's ultrasound training will prove to be a huge tool in the PRC tool-belt as more qualified medical professionals are learning the ultrasound skills they need to be successful in the collective quest for life.
 |
| RDMS trainer Barb Sheriff (Trisonics) with PHI Student Sue Rowland |
 |
| “In just a few short days these educators have filled me with more confidence than I thought I was going to finish this training with!” “I got an excellent foundation at this training.” |
 |
| PHI Student Peggy Rate, MD with RDMS trainer Sophie Calcara |
Ultrasound CME Course for Your Medical Director
Recognizing the great service your Medical Directors give to your centers, Heartbeat International also wants to support them in their mission. Please pass on the information below about a great opportunity to your Medical Director.
The AIUM American Institute of Ultrasound in Medicine is presenting
Gynecologic and Early Obstetric Ultrasound---- Solving Problems With Imaging
Register today for Gynecologic and Early Obstetric Ultrasound---- Solving Problems With Imaging. This course is brimming with essential, illuminating sessions such as:
- Why Should Ultrasound Be First for Imaging of the Female Pelvis? An Overview
- Adnexal Masses: When to Call an Oncologic Surgeon
- Procedures for Evaluating the Uterine Cavity and Tubes With Ultrasound
- How and When to Do 3-Dimensional Ultrasound Examinations
- The Many Faces of Endometriosis
- The Pelvic Floor: How to Evaluate It and Findings
Join Course Chair Beryl Benacerraf, MD, FAIUM, AIUM president, and other esteemed faculty September 25-26, 2015, in Las Vegas, Nevada. This course offers up to 11 AMA PRA Category 1 Credits™ (accepted by the ARDMS) or ARRT Category A Credits. Learn more here.
New FDA Consumer Update Urges Women to Obtain Medical Sonograms with Trained Operators
By Susan Dammann RN
The FDA has issued a warning. While the FDA's main focus in the warning is to advise pregnant women to avoid commercial sonogram services for nonmedical purposes that could pose a danger to the developing fetus, emphasizing that these are prescription medical devices, are to be used only by trained health care professional and only with a prescription, included within the warning are guidelines/recommendations which we in the pregnancy help medical clinics should be aware of.
Below are three excerpts from the 12/16/14 FDA Consumer Update which may pertain to the use of ultrasound imaging in the PMC, and a question for you to consider.
"Fetal ultrasound imaging provides real-time images of the fetus. Doppler fetal ultrasound heartbeat monitors are hand-held ultrasound devices that let you listen to the heartbeat of the fetus. Both are prescription devices designed to be used by trained health care professionals. They are not intended for over-the-counter (OTC) sale or use, and the FDA strongly discourages their use for creating fetal keepsake images and videos."
Question: Are the sonograms in your center being performed by trained health care professionals?
"The long-term effects of tissue heating and cavitation are not known. Therefore, ultrasound scans should be done only when there is a medical need, based on a prescription, and performed by appropriately-trained operators."
Question: Are the sonograms performed in your center based on a prescription for a medical need?
"Similar concerns surround the OTC sale and use of Doppler ultrasound heartbeat monitors. These devices, which are used for listening to the heartbeat of a fetus, are legally marketed as "prescription devices," and should only be used by, or under the supervision of, a health care professional."
Question: If your center uses Doppler, is it being used under the supervision of a health care professional?
As you consider the above FDA recommendations in relation to the ultrasound services performed in your PMC keep in mind also that one of the points in the Commitment of Care and Competence to which all Heartbeat Affiliates sign in agreement is:
Medical services are provided in accordance with all applicable laws, and in accordance with pertinent medical standards, under the supervision and direction of a licensed physician.
To read the full FDA Consumer Update click here.
Ultrasound Safety – Revisited
by Kevin T. Rooker, RT(R), RDMS, RVT, Sonography Consultants
Is ultrasound safe? Will it hurt my baby? These are questions we sometimes hear from our clients. We need to be able to answer those questions with confidence for several reasons. First, because our patients deserve an honest answer, and second because we never know who is listening. We know that there are some that think you should not be performing limited OB ultrasound and will always be looking for reasons to justify their position. Let's not give them that opportunity on the issue of ultrasound safety. Unfortunately, we, the medical community, have not done as well as we can at educating ourselves on the safety of ultrasound1.
Ultrasound is a wave of mechanical energy that penetrates human tissue as an oscillating (alternating) wave of high and low pressure. As it does so, there are two potential types of biological effects; Mechanical and Thermal. In 1993, the FDA allowed ultrasound manufacturers to significantly increase the amount of ultrasound energy created in diagnostic ultrasound systems, as long as they displayed the MI (Mechanical Index) and TI (Thermal Index) on the screen for the operator (and our clients) to see. The premise being that if we know what the MI and TI are, what their limits are, and most importantly how to lower them, then we are being as safe as we possibly can.
The Mechanical Index is a safety metric which lets the operator know how much energy is being transmitted into the patient during a sonography examination. Remember that sound is created by pressure waves, so mechanical energy is transmitted into any object which receives sound. Sound waves can be quite powerful. For example, think of the thump on your chest when sitting next to a teenager's car with the high dollar stereo system. It is defined as the peak negative pressure (PNP) of the ultrasound wave (point of maximal rarefaction). In easier terms; think pressure change divided by time. Lots of pressure change over short periods of time can be damaging. The FDA has established a maximum MI of 1.9 for diagnostic imaging. Any machine capable of generating MI greater than 1.0 must display the MI onscreen. The FDA MI limit for obstetric sonography is 1.0.
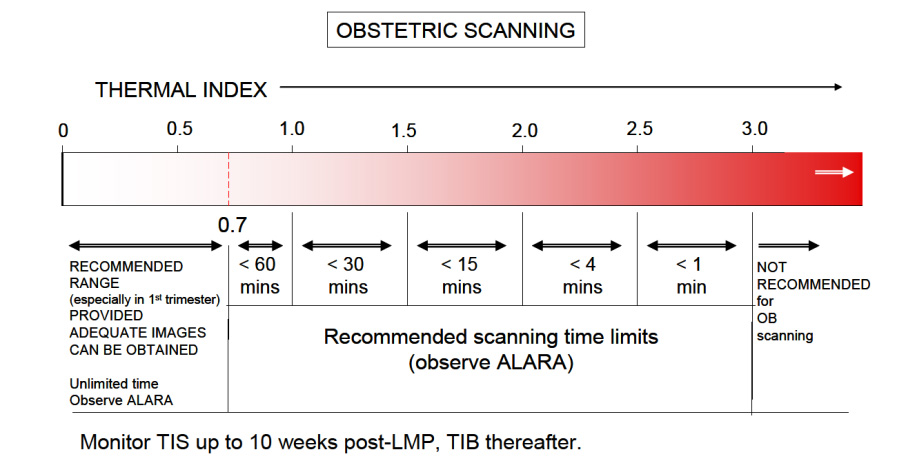
The Thermal Index is another safety metric which lets the operator know the potential of creating heat (hyperthermia) with the ultrasound beam. Many assumptions are made in this calculation, and it is often thought that the heating potential is underestimated. So keep in mind that the TI formulation was not intended to, and cannot provide an accurate measure of temperature rise within a specific patient. Instead it was designed to provide the operator with a relative measure of risk for a particular imaging mode. A Thermal Index of one (TI 1) indicates conditions under which the rise in temperature would be likely to be 1°C. The thermal index is different for different types of tissue, and can be displayed on your system accordingly: soft tissue (TIs), bone (TIb) and cranium (TIc). In the first trimester, when using Doppler to hear and demonstrate the fetal heart, the TIs setting us used. The limit for TI varies with time, please reference the chart below from the British Medical Ultrasound Society, the entire document may be found here.
Enough about what the MI and TI are, how do we as operators keep them at safe levels? There are two basic concerns to remember.
First is the AIUM ALARA policy2; which is an acronym for As Low As Reasonably Achievable. Simply translated, it means to keep the output power settings as low as possible, that still allows for adequate images. Most ultrasound systems can operate with output power settings at about 50% and still produce quite satisfactory OB images. Have your system presets adjusted so that when you are performing OB sonography both (abdominally and transvaginally), the output power settings are set low. You can always increase them if clinically necessary. And keep in mind that you can increase the gain to make your image brighter, as gain is just how well the system is "listening", it has no effect on the TI.
The second concern is time. Keep the overall examination as short as is reasonable. If using Doppler to allow Mom to hear her baby's heartbeat, depending upon your ceter's policy, keep the Doppler exposure to about 5-10 seconds. Know where to find the MI and TI displays on your system. If you don't know, consult your operator's manual or contact the manufacturer of your ultrasound system for more information.
Diagnostic ultrasound in obstetrics has been around for the better part of 40 years. To date, no one has been able to prove (and many have tried) that diagnostic ultrasound, when used prudently (MI,<1.0 and TI<0.7), has had any adverse effects developing fetuses; and this includes the limited use of Doppler in the first trimester "Thus far, there have been no significant thermal effects documented in humans and at this time the possibility of having all the factors present to is highly unlikely 3." However, it has been shown that aborting a living fetus is fatal, every time.
References
1. Ultrasound Is Safe . . . Right? Resident and Maternal-Fetal Medicine Fellow Knowledge
Regarding Obstetric Ultrasound Safety. J Ultrasound Med 2011; 30:21–27
Sheiner E, Abramowicz JS. Clinical end users worldwide show poor knowledge regarding safety issues of ultrasound during pregnancy. J Ultrasound Med. 2008;27(4):499-501
2. As Low As Reasonably Achievable (ALARA) Principle Approved 4/2/2014 aium.org/officialStatements/39
3. FDA Recommendations for the Safe Use of Ultrasound in Obstetrics CNE article authored by Sherri A. Longo, M.D. Assistant Professor in the Department of Obstetrics and Gynecology, Division of Maternal-Fetal Medicine, Tulane University School of Medicine in New Orleans, Louisiana; e-edcredits.com/nursingcredits/article.asp?testID=29
24 Hour Turn-Around on Ultrasound Scans?
Making Sense of AIUM Guidelines
Connie Ambrecht RDMS, Executive Director Equip Leaders Now/Sonography Now
Beverly Anderson, J.D., CEO Dove Medical
Susan Dammann RN LASm Medical Specialist
The Issue
In April 2014, the American Institute of Ultrasound in Medicine (AIUM) sent an email to its members stating it had "Updated Guidelines and Official Statements." Included in the list was the guideline titled "Documentation of an Ultrasound Examination."
First, it is valuable to revisit who AIUM is, as well as its role in ultrasound imaging. In its own words, "the AIUM is an association dedicated to advancing the safe and effective use of ultrasound in medicine through professional and public education, research, development of guidelines, and accreditation."
In the first section of the guidelines, AIUM outlines what it considers high-quality patient care. The guidelines state a permanent record should always be kept of the images, and an interpretation should be provided for patient records. All medical professionals involved should be able to communicate well and work as a team to provide what is expected: quality patient care.
The next section lists what should be included in the official report. In some clinical settings, the interpretation of the images is transcribed and a separate report page is generated for the patients chart. In the PMC setting it is common that a signature is obtained on the ultrasound report page and serves as the final report.
Section three discusses the final report from the interpreting physician or medical director of the clinic. According to this April 2014 update, the final report should be generated in 24 hours. I know you are thinking or asking... "How can we do that?!"
We restate the following from the AIUM guideline: Practice guidelines of the AIUM are intended to provide the medical ultrasound community with guidelines for the performance and recording of high-quality ultrasound examinations. The guidelines reflect what the AIUM considers the minimum criteria for a complete examination in each area but are not intended to establish a legal standard of care.
This AIUM Guideline is NOT a legal requirement. It is a national practice standard.
We at Sonography Now live in the service trenches with you as we train on-site. We understand that getting interpretations in a timely fashion versus every 24 hours can seem unnecessary. Taking one step at a time can ease such a transition. If you want to make changes to accommodate a faster interpretation time, it doesn't need to change immediately.
Building a plan of action can remedy the feeling of urgency. Some clinics we work with have images interpreted daily so that the final report can be given to the patient. You have the freedom to choose your course of action based on your mission and vision.
Concerning our routine ultrasound report procedure, we need to answer the questions:
- Do they jeopardize patient safety?
- Are they legally defensible?
- Would they put our reputation at risk if widely known?
Our patients feel an urgency to have definitive information about their pregnancy. They need their confirmed diagnosis, not the nurse's preliminary findings.
My nightmare concerning delays in the physician reading Dove Medical's ultrasound exams is that our nurse will miss an ectopic pregnancy the physician would have caught, the patient will not have received the appropriate instructions and/or referral for immediate care, and the patient will suffer injury as a result. I strive to insure both the skill level of our nurses and also the prompt reading of all exams.
Should We or Shouldn't We?
While some Medical Directors feel it would be consistent with the highest level of care which we strive for, that these standards should be recommended/set and then the center should work toward them, other Medical Directors who have discussed the issue feel strongly that we do not need to comply with the 24 hour mandate and that it would be impossible for most centers to do so.
Where the Rubber Meets the Road
We must remember that our Medical Directors are volunteering their services. If pressure is put upon them to comply with this standard, are we risking losing them as a Medical Director? If that scenario is a high probability, we must ask "How is this patient best served?" What do we tell the patient?
We can't do the sonogram because we can't turn the report around in 24 hours? Is a longer turn around period better for the patient than having no service at all? Also it is critical that we not alienate our Medical Directors who are sacrificing their time and skills to serve the patients in our clinic. Without them, we cannot offer ultrasound services at all.
If we set this as policy because it meets national standards but we cannot comply, what are the consequences? Is it better to adopt a policy set on the highest excellence we are feasibly able to provide so that we can continue serving our patients, rather than potentially losing our medical director or other consequences which would impede serving the patient? Then as we can, going forward, do what is possible to shorten the turn-around time.
Practical Considerations
Centers should make efforts to have ultrasound reports read, signed and returned within the shortest time frame that is reasonably feasible. Any scans with questionable findings of concern or emergency problems should be referred promptly to a physician or hospital emergency room. This policy should be made known to the patient on the intake form.
You may want to consider the following options, among others, as means to improve your turn-around time. This is only a sampling of options and not a recommendation of any specific option.
- Use Doc-U-Sign as a mechanism to transmit scans via internet with appropriate safeguards for patient identity.
- Both E-Kyros (www.ekyros.com) and WayCool (www.waycoolsw.com) have options available for uploading and securing the physicians signature.You may contact these businesses for more information.
- Some centers are using an encrypted cloud-based means of submitting their ultrasound reports to their physician or radiologist for review and signature.
- E-mailing the reports to the Medical Director using only a client number.
- Some ultrasound machines have a software program already installed that is capable of electronic transfer.
- Logmein is being used by some centers. This allows the Medical Director or Radiologist to log in to your computer via remote access from anywhere to sign reports. This requires transferring the images from your machine to your computer and either typing the report or scanning it in.
- Some centers upload scans to a memory stick, transfer them to the computer and use High Tail to send the ultrasound and reports to the Medical Director.
Consideration for Your Center
Inform your Medical Director of the recommendation by the AIUM and have a conversation with them. Let him/her know that it is a practice standard, not law. Discuss the best and most feasible policy for your center. Examine your current policy and practice – how well is that working? Does it meet the goal for the best service your clinic can provide for the patient? Look at and discuss some of the options for improving the turn-around time. Are there any steps you feel you should take at this time? Set a time to re-examine and evaluate.
General Ultrasound Checkup
The AIUM Official Statement concerning Limited Obstetric Ultrasound (LOU), reaffirmed on 4/2/2014, makes some clear statements about the services we provide. I am reminded again that we must see ourselves as competent medical professionals and our services as medical diagnosis. Points of emphasis in the AIUM Official Statement include:
- "A limited obstetric ultrasound examination is performed to answer a specific, acute clinical question." In our clinical setting a standard sonogram is unnecessary. Our clinical question is "Is there a viable pregnancy?"
- "Clinical judgment should be used to determine the proper type of ultrasound examination to perform." This is why we don't perform a LOU if the patient is bleeding or cramping. It is no longer clinically appropriate. We need to be absolutely clear in our messaging and in the statements made by staff that an ultrasound exam is performed only when clinically indicated. At Dove Medical, we no longer allow patients to schedule an appointment for an ultrasound. Our nurse offers an ultrasound when indicated and will schedule the exam for a later date if necessary. The patient can refuse an ultrasound, but she cannot demand one.
- "Lack of qualification or inexperience of the sonographer/sonologist does not justify performance of a limited ultrasound examination when a standard examination is indicated." Our nurses must tell the patient we obtain only three pieces of information because that is how we answer the specific clinical question before us. This means our RNs don't tell patients that they aren't trained to do [fill in the blank – patient questions we've gotten include "Is everything all right?" "Is it a boy or girl?" etc.]
- "Obstetric ultrasound examinations are not performed for entertainment or for sex determination in the absence of an accepted clinical indication." At PMCs, we perform the LOU to make a pregnancy diagnosis and for no other purpose.
- "When a patient undergoes a limited ultrasound examination, it is important that she understands why a limited scan is being done and that she has appropriate expectations regarding the information sought." Again, we must clearly understand the clinical reason we scan, so that our messaging to our patients emphasizes our scope of practice. Our consent form must have a statement about the limited exam to determine only three pieces of information (location of pregnancy, heartbeat, gestational age) for the purpose of diagnosing pregnancy because that is our limited scope of clinical practice and the patient must sign that she understands this.
As an education organization Equip Leaders Now and Sonography Now have responsibility to keep ourselves informed of changes that may impact your specialized clinical setting. Our role is to pass information along and let you decide how it fits in your clinic. At Sonography Now, our mission is to provide education related to imaging, at Equip Leaders Now, our mission is to build leaders by providing the tools needed to make informed decisions to build strong communities. In doing this we have an obligation to give you information so you can be empowered with the information to form your own talking points and messaging so you can be represented well in your community and to the patients you serve.
Contact Connie Ambrecht or Beverly Anderson at 702-925-8737 with any questions or for a private webinar for your team on this topic.
How Your Center Can Help Prevent Ebola's Spread

As the Ebola outbreak has spread from West Africa to isolated cases in parts of Europe and now the United States, there has been no shortage of panic and paranoia among Westerners—even those working in the health care fields.
Still, it is an established and repeated fact that Ebola's spread can be prevented simply by following proper safety procedures in a medical setting. An informational page on Ebola published at the World Health Organization's (WHO) website points to the sad reality of Ebola's largely preventable spread:
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD [Ebola Virus Disease]. This has occurred through close contact with patients when infection control precautions are not strictly practiced.1
As those involved in the life-saving work of pregnancy help in the medical setting, how can you protect yourself, your clinic, and your clients from this deadly virus?
The answer starts with educating yourself, your staff and volunteers, and your clients as to how Ebola spreads, which, again according to WHO, involves the following:
Ebola... spreads through human-to-human transmission via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.2
Consider the functions of your Pregnancy Help Medical Center or Clinic.
- Could you come into contact with any bodily fluid when handling a urine pregnancy test?
- What about collecting a specimen for STD/STI testing?
- Broken skin that can be exposed and contacted while conducting an ultrasound?
With these points of contact posing risks in light of the Ebola virus—in addition to several diseases that are much more likely to spread—make sure your center is paying special attention to policies such as Universal Precautions as defined by the Centers for Disease Control (CDC) and OSHA Regulations.
Under Universal Precautions, blood and certain body fluids of all patients are considered potentially infectious for HIV, (Hepatitis B), and other blood-borne pathogens. Universal Precautions involve the routine wearing of gloves, other protective clothing, hand washing, and such infection control measures that are designed to place a barrier between potentially infectious blood or body fluids and employees.3
For more information on how you can keep your center protected from the spread of viral infection, check out Heartbeat International's Medical Essentials for Pregnancy Help Organizations©.
1. "Ebola virus disease," World Health Organization, http://www.who.int/mediacentre/factsheets/fs103/en/ (accessed Oct. 17, 2014).
2. Ibid.
3. Medical Essentials for Pregnancy Help Organizations©, Heartbeat International, 2014, Part IV, page 4.
When am I Due? Why Should I be Concerned?
Healthy Pregnancy/Healthy Baby Series: Part 1
By Helen Risse RN MSN
 If you work with pregnant women, you have a great opportunity to improve birth outcomes. When a new client visits your pregnancy help organization, this may be the only contact you have with her.
If you work with pregnant women, you have a great opportunity to improve birth outcomes. When a new client visits your pregnancy help organization, this may be the only contact you have with her.
What should she be sure to know before she leaves you? Does she know her due date? Will you be telling her based on the first day of her last menstrual period?
It is important to define due date and term pregnancy. Remind your new mother that her due date is really a due time that looks at two weeks before to two weeks after that date as being "term". Many people still think of pregnancy in terms of nine months. Explain that pregnancy is defined as 40 weeks or 10 lunar months.
At the end of 2013, the American College of Obstetrics and Gynecology (ACOG) redefined the meaning of "term".
- Early term: Between 37 weeks, 0 days and 38 weeks, 6 days.
- Full term: Between 39 weeks, 0 days and 40 weeks, 6 days.
- Later term: Between 41 weeks, 0 days and 41 weeks, 6 days.
- Post term: Between 42 weeks, 0 days and beyond.
Research has noted that the brain of a baby at 35 weeks, 0 days grows in size by two-thirds in the following four weeks.
Research has noted that although the weight of a baby may look normal, babies born before 39 weeks are sleepier babies. These babies do not latch and suckle as well as babies born at 39 weeks 0 days. They have more problems with higher bilirubin levels. These concerns can lead to serious consequences. The choice of an elective delivery date must factor in these findings.
Women should also be taught the signs of preterm labor. Teach women about contractions. Explain what they may feel and describe those symptoms that should put them on alert.
Describe contractions as feeling like:
- Menstrual cramps
- Low, dull backache
- Pelvic pressure—feeling that the baby is pushing down
- Heavy feeling in your pelvis (pelvic congestion)
- Stomach cramps—with or without diarrhea
- The abdomen may tighten or get firm then relax or soften
Describe vaginal discharge or bleeding:
- An increase or change in your normal vaginal discharge
- Red, brown or pink discharge or spotting
Describe water breaks:
- Gush of fluid from vagina
- Slow trickle of fluid from vagina-(panties feel wet and you don't know why)
General feeling that something is not right.
What should she do if she thinks she may be having preterm labor? Below are some guidelines you may discuss with your Medical Director to develop a policy/procedure for your center.
- Empty bladder
- Drink 1-2 glasses of water or juice (no caffeine, sugar, or sports drinks)
- Lie down on your side and time the contractions from the beginning of one to the beginning of the next. Write down when the contractions start.
If the contractions are coming more than every 15 minutes or 4-6 in an hour, call your doctor.
It is important to stay well hydrated. Dehydration can often cause a woman to experience contractions.
Women should know the risks that increase concerns for preterm labor. Women who are at greatest risk for preterm labor are those who have had a previous preterm birth, as well as those who are pregnant with multiples, and those with certain abnormalities of their uterus or cervix.
Other risk factors include smoking, drinking alcohol, using illegal drugs, domestic violence, including physical, sexual or emotional abuse, or lack of support.
Additional risks factors related to her health include infections, including urinary tract infections, sexually transmitted infections, diabetes, high blood pressure, second trimester bleeding from the vagina, being underweight before pregnancy, obesity, and a short time period between pregnancies.
When asked if there is anything that can be done to prevent preterm labor, tell a woman to:
- See her doctor early and regularly during pregnancy,
- Eat nutritious meals and snacks,
- Drink at least 8 glasses of water, juice or milk every day, and
- Avoid cigarettes, alcohol, drugs and medications not prescribed by her doctor.
If you have one visit from a pregnant woman and pass on this information, you may contribute to an improved outcome. Every extra day her baby is in a healthy intrauterine environment is positive for the development of her baby, which in turn can be a big help to a new mother.
References
Spong CY. Defining "Term" Pregnancy: Recommendations From the Defining "Term" Pregnancy Workgroup. JAMA. 2013;309(23):2445-2446. doi:10.1001/jama.2013.62
ACOG Clinical Guidelines: Definition of term pregnancy. Committee Opinion No. 579. American College of Obstetricians and Gynecologists. Obstet Gynecol 2013;122:1139–40.35
Go the Full 40 Campaign tool Kit :http://www.health4mom.org/pregnancy/healthy_pregnancyo
The last weeks of pregnancy count: July 5th, 2012l Kit: http://newsmomsneed.marchofdimes.com/?tag=brain-development



