Displaying items by tag: medical
What are Standing Orders and Are They Legal?
By Martha L. Teter MS, CRNP
 |
Many states in the United States have laws and rules regarding the use of “standing orders” or protocols for non-prescribers to administer medications. Do you know what the laws in your state are? Heartbeat International strongly recommends that you research your state laws in this area and be sure you are in compliance with them if you are operating in any area according to standing orders for the administration of treatment or medication, such as in the area of STD/STI treatment.
As an example, in the State of Ohio, no medication may be given to any patient without prior assessment of the patient’s condition by a legal prescriber and documentation of the legal prescriber's order on the patient's record.
Legal prescribers in the State of Ohio, include Physicians, and the following Advanced Practice Nurses who also hold Certificates to Prescribe: Certified Nurse Practitioners, Certified Nurse Midwives and Certified Clinical Nurse Specialists. Many Certified Physician Assistants also have Certificates to Prescribe and are legal prescribers.
A standing order or protocol is a definitive set of treatment guidelines that include definitive orders for drugs and their specified doses. These “Standing Orders” have been authorized by a prescriber to be administered by a certified or licensed health care professional, to a patient for a specific condition. This type of “Standing Order” or Protocol may only be utilized by licensed health care professionals in Ohio in the following situations.
- Emergencies
- Administration of biologicals for the purpose of disease prevention, and
- Administration of vaccines for the purpose of preventing disease
The administration of drugs for any reason other than the above exceptions and that are not patient specific or authorized by the prescriber prior to implementation would be the unauthorized practice of medicine, which is a felony in the state of Ohio. The details of how and when the above exceptions may be applied are detailed in Ohio law.
If you would like to learn more about Ohio Law regarding standing orders, click here.
Many other states also have laws regulating standing orders. To learn more about the laws in your state, log onto the professional websites of The State Board of Nursing, The State Board of Medicine or the State Board of Pharmacy. Should you find that your current practices are not in compliance with your state law, Heartbeat International recommends that you place a hold on further treatment until such time as you can assure you are in compliance with your state law.
If you have any further questions please feel free to contact Heartbeat International.
Get up to Speed on Ectopic Pregnancies
|
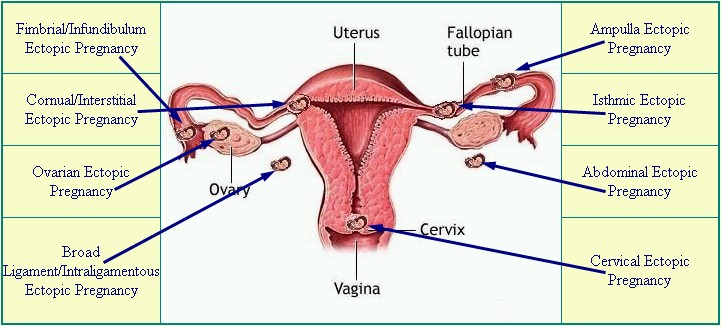
Diagram from EctopicPregnancyFoundation.org |
By Susan Dammann, RN, Medical Specialist
Ectopic pregnancies occur in a range of 1 in 40 to 1 in 100 pregnancies. An ectopic pregnancy is any pregnancy that implants somewhere outside of the uterus, most often occurring in one of the fallopian tubes, which is also known as a tubal pregnancy. Other locations for an ectopic pregnancy include the ovary, the cervix, and the abdominal cavity.
Ectopic pregnancies are life-threatening for the mother, and the baby (embryo) cannot survive. Ectopic pregnancies may occur with or without the use of birth control.
Though rare when considered with the overall number of U.S. pregnancies, ectopic pregnancies still occur at a rate of 100,000 per year, according to the Center for Disease Control. The CDC also reports the life-threatening nature of an ectopic pregnancy for a mother: "Ectopic pregnancies are the leading cause of pregnancy related deaths in the first trimester and account for 9% of all pregnancy related deaths in the country."
Causes
An ectopic pregnancy can result from any condition blocking or slowing the movement of the embryo through the fallopian tube, where it then becomes lodged. The cause, sometimes unknown in an individual case, may include any of the following:
- Tubal damage resulting from sexually transmitted infections
- Inflamed, damaged or misshapen fallopian tube
- Hormonal imbalances
- Abnormal fetal development
- Complications/scarring after a ruptured appendix
- Endometriosis
- A previous ectopic pregnancy
- Scarring from past infections or surgery of the female organs
- Illicit drug use (“An alarming increase in ectopic pregnancy-related deaths among Florida women is likely caused by illicit drug use and delays in seeking medical care…”)
Risk Factors
- Having had many sexual partners
- Surgery to reverse a tubal ligation
- IUD in place
- In vitro fertilization
- Over 35 years of age
- Some infertility treatments
- Tubal ligation (more likely 2 or more years after the procedure)
Symptoms
Initially, an ectopic pregnancy may not cause any symptoms outside of those of a normal pregnancy. A pregnancy test will read positive, but will likely be accompanied by the following symptoms:
- Abnormal vaginal bleeding—heavy vaginal bleeding is not likely unless the ectopic pregnancy is in the cervix
- Pain in the lower belly or pelvic area
- No period
- Low back pain
- Cramping on one side of the pelvis
If the areas around the ectopic pregnancy rupture and bleed, symptoms may worsen and include:
- Low blood pressure
- Pain in the shoulder area, due to blood leaking from the fallopian tube
- Urge to have a bowel movement, due to blood leaking from the fallopian tube and pooling
- Severe, sharp, and sudden pain in the lower abdomen
- Fainting or feeling faint
Complications
- Unless treated, a ruptured fallopian tube may be life-threatening
- Shock
- Infertility
Diagnosis
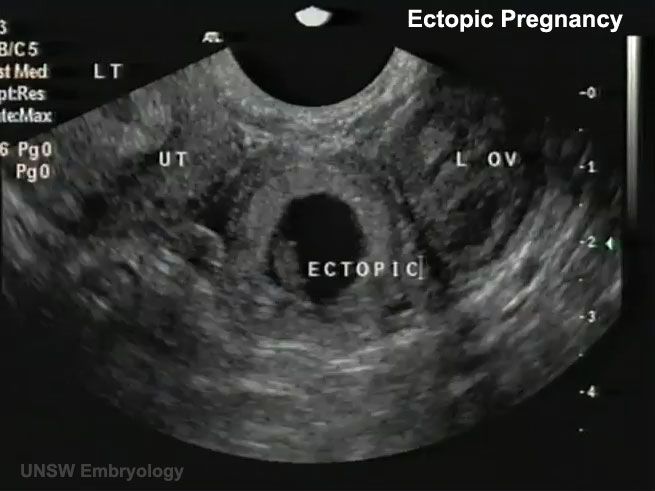
If an ectopic pregnancy is suspected, the physician may do a pelvic exam to check for pain. Tenderness or a mass in the fallopian tube or ovary may be an indicator. Blood tests and vaginal ultrasound exam help confirm the diagnosis, as does checking hCG blood levels over 1 to 2 days.
[Related—Transvaginal Sonogram: Is it Necessary in Your Center?]
Ectopic pregnancy may occur after tubal ligation, even more so if the woman was sterilized before 30 years of age. One study found these women were twice as likely to have a subsequent ectopic pregnancy as those women who undergo tubual ligation after the age of 30. It should never be assumed that a woman’s history of tubal ligation automatically rules out the possibility of an ectopic pregnancy.
Treatment
In order to prevent the loss of a mother’s life in addition to the loss of her embryo, intervention is required. The pregnancy cannot continue to full-term. If the ectopic pregnancy is diagnosed before symptoms occur, treatment may consist of an injection of methotrexate to stop cell growth. Ectopic pregnancies can be removed through laparoscopic surgery. If the fallopian tube is damaged, it may need to be removed as well.
Emergency medical attention is required if the fallopian tube has ruptured and heavy bleeding is occurring. Emergency surgery (laparotomy) may be required to stop the blood loss, as well as the termination of the pregnancy and possibly removal of the fallopian tube. Because the rupture can lead to shock, the following may be necessary:
- Blood transfusion
- Intravenous fluids
- Oxygen
- Trendelenberg position
- Added warmth
Prognosis
While some women do not conceive subsequent to an ectopic pregnancy, approximately one-third do experience a later pregnancy. Of this one-third who do become pregnant following an ectopic pregnancy, approximately one-third will have a repeat ectopic pregnancy.
Prevention
The best means of avoiding a tubal pregnancy is to avoid anything that would cause infection, or scarring of the fallopian tubes. Early diagnosis and treatment of all STD/STIs is critical. There are, however, no preventative measures to avoid ectopic pregnancy occurring outside the fallopian tubes.
Patient Instruction Sheet
This information is critical for pregnancy center staff to know. With every client who comes in our center with a positive pregnancy test we must be aware that she could potentially have an ectopic pregnancy. Therefore, it is recommended every center have a policy and procedure for advising clients of the signs and symptoms of an ectopic pregnancy.
This could be as simple as giving your client a sheet of instructions and information listing the signs and symptoms of an ectopic pregnancy, along with instruction to contact a health professional immediately if she experiences any of these symptoms.
Sources:
1. http://www.mayoclinic.com/health/ectopic-pregnancy/DS00622
2. http://www.nlm.nih.gov/medlineplus/ency/article/000895.htm
3. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001897/
Tubal pregnancy; Cervical pregnancy; Tubal ligation-ectopic pregnancy
4. CDC Fact Sheet: Ectopic Pregnancy Risk after Tubal Sterilization
[CDC Reproductive Health Information Source, 7/04 http://pregnancy.about.com/cs/ectopicpregnancy/l/bltubalfacts.htm]
5. http://health.usnews.com/health-news/news/articles/2012/02/16/illicit-drug-use-may-be-driving-rise-in-ectopic-pregnancies-in-florida
Transvaginal Sonogram: Is it Necessary in Your Medical Center?
by Audrey Stout, RN, RDMS, SoundView Imaging Partners
 |
In over ten years of educating abortion-vulnerable women on fetal development and abortion, I had seen many of these women experience a change of heart. Yet, for years, I also believed that if a woman was able to see her unborn child through ultrasound, many more would choose life. From the very beginning, we knew transvaginal ultrasound to be the best means of imaging a pregnancy in the early stages.
One objection we may not have anticipated was this: “We don’t want to do that, do we? What if the girls have not had a bath before coming?” Our medical team appropriately determined that we must “do that,” and then learned to perform both abdominal and transvaginal ultrasounds in order to provide pregnant women with services equal to the standard of care in the broader medical community.
Even with more than 600 pregnancy medical clinics offering medically indicated limited OB ultrasounds, there is still a lack of a common understanding for the necessity of transvaginal ultrasound in the pregnancy medical clinics, which bears itself out in resistance or hesitance to utilize this valuable resource. But transvaginal sonograms are absolutely necessary for pregnancy medical clinics.
The Importance of Transvaginal Ultrasound
For early pregnancies, as well as women with a retroverted uterus or obesity, the use of transvaginal sonography is critical to determine the location of the pregnancy, since the child is tiny, and often not visible when scanning abdominally.
During a recent training involving around 60 scans, there were two patients for whom it was impossible to determine if there was a true gestational sac or pseudo sac of an ectopic pregnancy in the uterus by scanning abdominally. When the transvaginal probe was used, however, both ultrasounds revealed tiny embryos with beating hearts, measuring from 2-3 mm (25 mm=1 inch) in length alongside a yolk sac—diagnostic for an intrauterine pregnancy.
Apart from using the transvaginal probe in each of these cases, the patients would have needed both ectopic and miscarriage precautions, due to an inconclusive ultrasound. This would have required a follow-up scan, either at the PMC or with another physician, for serial hCG levels, in addition to another sonogram to rule out an ectopic pregnancy. This would have caused needless stress and concern, when the answers were available with a transvaginal scan. When a woman seriously considering abortion comes into a pregnancy clinic, we may only have one opportunity to see her and provide a life-affirming sonogram.
The three medical indications, for performing a limited OB sonogram in most PMCs according to the American Institution for Ultrasound in Medicine:
- To confirm the presence of an intrauterine pregnancy.
- To confirm cardiac activity.
- To estimate gestational age (EGA).
From the Textbook to the Pregnancy Medical Center
Every woman considering abortion needs this information to make a truly informed choice regarding her pregnancy. Using transvaginal sonography during the first trimester, one is much more likely to be able to answer the three questions listed above, and enable a woman to see the life of her unborn child in order to refute the idea that her child is just a mass of tissue.
PMCs typically see women in early pregnancy when they are most likely to have ectopic pregnancies, as most show symptoms between 7-8 weeks LMP. Since a ruptured ectopic pregnancy is life-threatening due to massive hemorrhage, every early sonogram must attempt to determine the location of the pregnancy. Ectopic pregnancy is the leading cause of first trimester maternal death, even though less than 9% of ectopics are actually visualized with a fetal pole on sonography because they are notoriously difficult to diagnose.
Skill in both transabdominal scanning and transvaginal scanning are necessary, as some ectopics or associated findings are visible with abdominal scanning, while most can only be visualized using transvaginal scanning. Transvaginal sonography also can uncover a rare condition known as “heterotopic pregnancy,” which is both intrauterine and ectopic, occurring at a rate of 1/30,000 in natural reproduction.
A recent article from MedPage Today discusses ectopic pregnancies and highlights the need for using transvaginal sonography. The article states:
Ectopic pregnancy occurs in up to 2.6% of all pregnancies and is the chief cause of first-trimester pregnancy-related mortality, accounting for up to 6% of maternal deaths. However, less than half of women with ectopic pregnancy have characteristic symptoms of abdominal pain and vaginal bleeding, which are more likely to indicate miscarriage.i
Further, ectopic pregnancy has been on the increase since 1970, when the Center for Disease Control began tracking this condition.
Key Factors to Keep in Mind
As those performing ultrasound services in the PMCs, adequate training is critical in order to gain skills in imaging the maternal anatomy, demonstrating with every sonogram that the pregnancy is intrauterine (IUP). If one does not possess these skills, it puts not only the woman who comes to you at-risk for losing her life, it also puts your PMC at legal risk of liability for harm. Thankfully, many women have been protected from life-threatening ectopic ruptures, due to the careful and skillful scanning of nurses and other medical personnel in PMCs.
Here are five tips to protect all involved by safely performing sonograms to the highest standard of medical care in your PMC:
- Attend a foundational didactic course for performing Limited OB Sonography in accordance to the Association of Women's Health, Obstetric and Neonatal Nurses Guidelines (AWHONN), e.g. the NIFLA course (NIFLA.org).
- Gain adequate hands-on training by an RDMS or physician skilled in performing OB sonograms to demonstrate competency in skills, both abdominally and transvaginally before performing sonograms without direct supervision. A minimum of 50 scans is strongly recommended for every sonographer, though for most, 60-75 may be needed. Documented competency is key to safety in scanning. Those skills should be assessed and refreshed on an annual basis.
- Follow a systematic scanning protocol, always beginning with an abdominal survey of the pelvis (including the adnexae and uterus) in two planes to identify the pregnancy location and get an idea of the gestational age.
- If with abdominal scan, one cannot clearly visualize anatomy (the vagina, cervix and contents of the uterus, i.e. gestational sac and fetal pole) with a high level of resolution to demonstrate an IUP, perform a transvaginal scan throughout the first trimester. When an IUP is not demonstrated, one must always suspect ectopic and provide precautions. Never assume it is too early.ii
- Consider sonography a life-long learning and skill journey, with excellence as the goal. For competency and skills growth, a sonographer should perform approximately 100-150 scans each year.
So, are transvaginal sonograms necessary in your PMC? Yes, yes, and yes.
Transvaginal sonograms safely provide sonography services and protect those served. In fact, sonographers with adequate training often happily admit, once they have acquired the skills, they very much prefer transvaginal scans because of the superior resolution and the fact that women are able to clearly see the image of their unborn child.
________________________________________
Audrey Stout, RN, RDMS, has a passion for the cause of life and began involvement with pregnancy centers in 1987. In 2000, she began instructing with NIFLA’s Limited OB Ultrasound Course and serves as National Nurse Manager Consultant for NIFLA as well. She has provided hands on trainings in sonography for PMCs medical personnel throughout the US, and is a founding partner with SoundView Imaging (SoundViewImaging.org). Audrey lives in Lexington, VA with her husband, Dave. They have three grown adopted children and one grandson.
Notes
i. Boyles, S. Transvaginal Ultrasound Best to Find Ectopic Pregnancy. April 23, 2013. Medpage Today. Accessed June 25, 2013 from: http://www.medpagetoday.com/OBGYN/Pregnancy/38638.
ii. Bourgon, D., Lin, E., Ectopic Pregnancy Imaging. April 12, 2011. Medscape. Accessed June 28, 2013 from: http://emedicine.medscape.com/article/403062-overview.
Response to CDC Report: Decline in State Teen Birth Rates by Race and Hispanic Origin
 |
This article was originally written by the Medical Institute for Sexual Health, received July 1, 2013. It is reprinted as written in its entirety with permission.
In May 2013, the CDC released the report Decline in State Teen Birth Rates by Race and Hispanic Origin.1 This report includes four important findings. First, the teen birth rates fell by at least 15% for all but two states during 2007 – 2011. In fact, seven of these states recorded a decrease of about 30% or more.1
Second, this decline in teen birth rates was most rapid in Hispanic teenagers who achieved a 34% reduction, followed by non-Hispanic Blacks at 24% and non-Hispanic white teens at 20%.1
Third, the recorded long-term difference between teen birth rates for non-Hispanic blacks and Hispanic teenagers had gradually disappeared over five years of follow-up data from 2007 – 2011, and the rates had become virtually identical for both groups in 2011, the most current year for which data is available.1,2
Fourth, the rates for Hispanic teens fell about 40% or more in 22 states and the District of Columbia.1 In all, rates for Hispanic teens decreased by at least 30% in 37 states and DC.1
Although this decrease has been attributed to an increased use of contraception (long acting reversible contraceptives (LARCs), oral contraceptive pills, and condoms) among teenagers;3 the number of teens who have initiated sexual intercourse or are currently sexually active has been on the decline.4 This trend has also been a contributory factor in decreasing teen pregnancies and consequently teen births. However; the rates of sexually transmitted infections have been on the rise among sexually active teenagers and young adults aged 15 – 24 years.5
Even with the record decline among all populations of teens; especially in minority populations, the work is not yet done in making sure this trend is sustained among teens of all ethnic groups. Focusing on sexual health education, character training, and parenting education at the community level are all initiatives that could address different needs of various populations within the US. Currently, the Medical Institute offers training to health educators and community liaisons to teach these topics to parents in a wide range of communities across the US.
Surveys continue to show that parents are very influential in the sexual decision making of their children but that parents are frequently unaware of this influence.5 Therefore, it is important for parents to be prepared to discuss these topics with their children. Increasing the involvement of parents in the sexual and character education of their children offers the opportunity to capitalize on the unique position of influence that parents hold and to deliver the message in an individualized, culturally-appropriate way.
We cannot underestimate the role of a number of social factors that influence the sexual behavior of teenagers. However, evaluation studies have shown a common thread in the positive effect of parental communication and connectedness in delaying sexual initiation and helping young people make healthy sexual decisions.6
The decline in teen birth rates is a welcome development. However, the STI rates among this population have been increasing. Working towards a reduction in the rates of other attendant negative outcomes of early sexual initiation such as sexually transmitted diseases and emotional consequences is also critical. Consequently, a risk avoidance prevention message continues to take priority in achieving this goal. Avoiding all risky behaviors is the most reliable way to prevent the myriad of adverse outcomes associated with such behaviors. By emphasizing risk avoidance messages; parents, parenting adults and educators can guide youth towards making the healthiest decisions and leading productive lives.
About Medical Institute for Sexual Health
The mission of the Medical Institute for Sexual Health is “To empower safe, healthy living by communicating objective and scientific sexual health information.” MI is focusing on five initiatives: Parent Education, Adolescent and College Education, Sex in Media, Medical Accuracy, and Medical Education. These initiatives will facilitate access to medically accurate, evidence-based sexual health information.” The Medical Institute offers a wealth of information and resources relating to sexual health. For additional information, visit https://www.medinstitute.org/.
References:
- Hamilton BE, Mathews TJ, Ventura SJ. Declines in state teen birth rates by race and Hispanic origin. NCHS data brief, no 123. Hyattsville, MD: National Center for Health Statistics. 2013. Available at: http://www.cdc.gov/nchs/data/databriefs/db123.htm . Accessed June 28, 2013.
- Hamilton BE, Ventura SJ. Birth rates for U.S. teenagers reach historic lows for all age and ethnic groups. NCHS data brief, no 89. Hyattsville, MD: National Center for Health Statistics. 2012. Available at: http://www.cdc.gov/nchs/data/databriefs/db89.htm . Accessed June 28, 2013.
- Martinez G, Copen CE, Abma JC. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2006–2010 National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat 23(31). 2011.
- CDC. Youth Risk Behavior Surveillance—United States, 2011. MMWR. 2012;61(No. SS-4). Available at: http://www.cdc.gov/mmwr/pdf/ss/ss6104.pdf . Accessed June 28, 2013.
- Satterwhite CL, et al. Sexually transmitted infections among U.S. women and men: prevalence and incidence estimates, 2008. Sex Transm Dis 2013; 40(3): 187-193.
- Albert, B. (2012). With One Voice 2012: America’s Adults and Teens sound Off About Teen Pregnancy. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy. Available at: http://www.thenationalcampaign.org/wov/ . Accessed June 28, 2013.
- Markham CM, Lormand D, Gloppen KM, Peskin MF, Flores B, Low B, House LD. Connectedness as a predictor of sexual and reproductive health outcomes for youth. J Adolesc Health.2010; 46(3):S23-S41.
Building on What We Have Done
Making Abortion Unwantable
by John T. Bruchalski, MD, FACOG

OUR PURPOSE
How can OBGYNs and Pregnancy Resource Centers (PRCs) collaborate to build a healthier community where abortions are unwanted? This is the purpose of this presentation. Seeing the benefits of what we have accomplished has been inspiring, but we can do more. Based on Tepeyac Family Center’s work of serving regional pregnancy centers in Northern Virginia for the past two decades, we have a few ideas on how to make abortion unwantable.
Individually, our purpose on Earth is to love God and love our neighbors with all of our heart, mind and soul. Faith and charity go hand in hand. As Tepeyac physicians, we see medicine as an act of mercy where we care for and have compassion for the sick and vulnerable, the “least of our brothers and sisters.” There is no better way to live this vocation as an OBGYN than by serving the local PRCs in our neighborhood, community, and beyond.
Compassion means to suffer with, and we can suffer with our clients and patients and love enough by working together. Practicing merciful medicine removes the reasons for abortion and does so much more than save a baby. We are working toward Transforming Hearts Through Healthcare™ and mercy shows God’s grace.
Let us elucidate the problems that OBGYNs face today, so we can suggest some practical answers to make abortion unwantable.
OUR PROBLEMS
Everywhere we turn, the world seems to be in crisis. With massive changes to the United States (U.S.) healthcare system, physicians today are more cynical, pessimistic, fearful and tired than I have seen in three decades of practicing medicine. The present government solution to fix healthcare decreases reimbursements to doctors and increases paperwork and overhead costs with complex regulations.
Moreover, the Affordable Care Act (ACA) has ignored the entire issue of malpractice resulting in increases in liability insurance costs. Under the rhetoric of “reproductive rights” and “women’s healthcare”, the current administration has enshrined abortion and contraception as mainstream medical practices despite the stigma, the paucity of providers, and split in public opinion.
Further, the ACA dismisses personal consciences and violates religious freedoms. The American Congress of Obstetricians and Gynecologists (ACOG) has assaulted conscience rights of future doctors and is demanding that their member doctors either refer or perform abortions. ACOG knows that most physicians refuse to perform the procedures because of its barbaric nature and the number of abortionists is dwindling.
Below are my observed problems that OBGYNs face in building relationships with crisis pregnancy centers and making abortion unwantable.
Problem #1: Lukewarmness
The first problem is lukewarmness. Lukewarm is a problem for physicians on both sides of the abortion issue. Sadly, I know this from first hand experience. I spent the first two years of my career as an abortion provider. Thankfully, my faith and prayer life led me to a place where I am no longer forced or required to violate my conscience. By faith and sacrifice, my wife and I founded Tepeyac Family Center in Northern Virginia in 1994, and its parent company Divine Mercy Care (DMC) in 2000.
My Tepeyac colleagues and I have worked alongside and inside pregnancy resource centers as volunteer counselors, advisors, and board members. Despite many excuses, the primary, honest reason most doctors do not perform abortions is the brutality of the procedure. Over one million abortions are performed in the U.S. annually and most doctors are simply not that passionate about abortion to actually perform them. It is easier for doctors to refer abortions out to the local abortionist.
On the pro-life side, most doctors, even those identified in a Christian faith tradition, are really not that passionate about the dignity of human life to take on the added malpractice risk of seeing women with crisis pregnancies, or accept the financial burden of caring for people without insurance. Providing life-taking or life-affirming care is too much of a burden to physicians with so many other problems and responsibilities to deal with on a day to day basis.
Lukewarmness among doctors is a problem for both sides of the abortion issue.
Problem #2: Idolatry
The second problem is chasing idols. My profession has placed idols before the source of happiness and joy. Idols include making money and increasing prestige; believing abortion is an answer to social and medical problems yet being lukewarm in its practice; not searching for the root cause of unplanned pregnancies; accepting rampant promiscuity and the resultant diseases that follow; treating fertility as a disease and children as sexually transmitted infections; pitting mothers and fathers against their unborn children; and working with suffering without seeing the redemptive nature when suffering cannot be relieved.
As doctors who have taken a vow to “do no harm” and care for all who come before us, physicians have moved away from His light and became instruments of evil in the world, subject to the worst of tyrannies. As OBGYNs, we are being asked to hold back from God and to hesitate to answer His call. Because we are fearful of the cost, the pain, the unknown, we no longer trust the Divine Physician nor do we care or serve our neighbors in need. This is the malice found in our soul.
We have become hollow, filled with emptiness and fear. Rather than turn to Christ, we grasp for more of the same: more abortion, more contraception, more sterilization and more secular, sexual education. When we attempt to follow ways other than willed by God, we find loneliness and sadness. We chase idols.
Physicians have stopped treating two patients; OBGYNs are being taught to treat a patient with a disease in her womb. No mercy and no care. Faith and love have gotten a divorce from each other and from ourselves, yet, we are called to care for women in crisis pregnancies and show her how to care for her unborn child. This is Tepeyac’s model of practicing excellent and merciful medicine. As a consequence of doctors being lukewarm and chasing idols, Heartbeat and your ministries heroically and sacrificially give of your time and expertise in meeting the needs of the woman with an unwanted pregnancy.
You are present at the time of crisis and need. But this is not enough. PRCs have to provide ultrasounds because doctors in your communities cannot meet this need.
The medical model of a pregnancy resource center was born out of necessity because we in the medical profession, for the most part, have turned our backs on caring for two patients by eliminating the humanity of the fetus and violating the dignity of the woman. Most doctors, even those of Christian faiths, only see the poor on sabbaticals and not during their daily work, when in truth, there are poor people living in our very own community that need our help. We allowed abortion to become a valid medical practice in the Affordable Care Act because we did not uniformly stand together voicing our outrage.
We abdicated the intellectual and scientific truth of when life begins.
With almost twenty years of experience, Divine Mercy Care (DMC) and Tepeyac Family Center offer a solution.
OUR SOLUTION
Abortion and healthcare are NOT political footballs at Divine Mercy Care and Tepeyac Family Center. DMC’s solution has seven practical principles resting on a solid three-pillar foundation of serving, inspiring and unifying when collaborating with PRCs. Nearly two decades of being on the front lines has taught Tepeyac doctors much about combating “lukewarmness” and “idols”.
#1. SEE PATIENTS
Tepeyac’s doctors have found a method through sacrifice, hard work and tithing for medical practices to see all patients; those insured and those not insured or under-insured by outreaching to all pregnancy resource centers in our region. Charity, not entitlement, is at the heart of serving our community. Every PRC is different, so we do not force anything on anyone. We offer our obstetrical expertise to care for the woman and the child in the hopes of helping her see the blessing of the child. We introduce her to resources intended to build a stable and strong family and/or support system. Our fiscal approach is called the MERCY Program where we financially cover medical services that the patient cannot afford. We want to be able to do more than save a baby; we introduce them to community services for a continuum of support; we work toward turning around a life and transforming hearts.
#2. HELP WITH ULTRASOUNDS
We recognize the great work many PRCs do with their medical model of providing ultrasounds to women in crisis pregnancies. Further, Tepeyac provides immediate ultrasounds and doctor visits for PRC patients. We are applying to open Tepeyac School of Sonography (TSS) Certification Program. If approved by the Commonwealth of Virginia, State Council of Higher Education, TSS will offer a 13-week curriculum designed to train your ultrasound technicians and ready them for the American Registry for Diagnostic Medical Sonography testing.
Medical care is more than a technical skill. Ultrasound technicians must meet the rigorous professional and safety standards while loving the patients, both mother and baby. This can be taught. Tepeyac shows students how to love and treat patients while fully complying with radiology standards. Additionally, Tepeyac’s standard of providing high quality ultrasound services in a supportive, life-affirming environment ensures that staff respond lovingly to patients who have an abnormal scan.
#3. CARE FOR THE LEAST
Our Kristen Anderson Perinatal Hospice Program is Tepeyac’s medical, spiritual and community approach to a woman carrying a terminally sick child. The hospice approach maximizes the time a mother spends with her preborn child and enhances the love available for the family as a whole.
#4. OFFER A MEDICAL DIRECTOR
By having a pro-life radiologist and OBGYNs at Tepeyac, we are able to electronically connect PRCs to a medical expert to read and interpret sonographic information. With the internet and open hearts, no distance is too far to provide excellent medicine and excellent resources.
#5. EDUCATING STUDENTS, RESIDENTS AND OTHER PROFESSIONALS
Leading by example, DMC, through Tepeyac, can help doctors in your area realize the critical importance of not simply sitting on boards, or counseling, but actually seeing the client in need as a patient and building relationships. To transform hearts and minds, we actively attract men and women who are pursuing healthcare degrees and help them understand the importance of working with PRCs once they enter private practice. This is not on top of what we do, this is what we do. Collaborating with PRCs is a way to give back to the community in your own neighborhood.
#6. INVOLVED IN RAISING MONEY
This is not a “zero sum” game. We cannot continue to the “turf wars.” We serve a generous God. DMC can speak at annual banquets to help inspire those in the audience to give generously to this most urgent of causes. When donors and financially savvy people see the cooperative nature of PRC with a medical practice and other services, they are apt to give more generously knowing that they are not duplicating life-affirming services.
#7. BREAKING DOWN WALLS
It is clear the prolife community needs to be more unified. This is easier said than done. Thankfully, Tepeyac’s approach seems to bring together doctors, PRCs, emergency rooms, maternity homes, social services, specialists, and even churches of various faith traditions. There is a way to live by example the axiom that we can love enough together to make abortion unwantable, children welcomed and families stronger.
Faith and charity is the goal of living. We can overcome the “lukewarmness” and the “idols” by working more closely together. OBGYNs and PRCs need to collaborate. The great work that Heartbeat International and Tepeyac Family Center have accomplished can be improved on, building on what we have done and making abortion unwantable. The above steps are the practical ways this can happen.
Please contact us for a conversation that can lead to the continuing transformation of hearts for our patients, clients and ourselves.
John T. Bruchalski, MD, FACOG Founder, Tepeyac Family Center
Chairman, Divine Mercy Care
11096-A Lee Highway, Suite 101
Fairfax, Virginia 22030 -5039
703-934-5552
This email address is being protected from spambots. You need JavaScript enabled to view it.
FDA approves morning sickness drug Diclegis
by Susan Dammann, Medical Specialist, LAS

On April 9, the U.S. Food and Drug Administration approved the morning sickness drug Diclegis, 30 years after it was pulled from the market due to concerns that it caused birth defects.
Diclegis is a delayed-release tablet, a combination of doxylamine succinate, an antihistamine, and pyridoxine hydrochloride, a form of vitamin B6, and is used to treat pregnant women who have not responded well to other means of dealing with morning sickness.
Although both substances have been prescribed separately for several years, this combination is an extended release formula, intended to stop the morning sickness before it begins. Sometimes the conservative treatment of eating smaller meals, eating low fat or bland foods which are easier to digest, and avoiding smells that can trigger nausea are not adequate in controlling the symptoms of morning sickness.
According to the FDA’s press release announcing its approval, the recommended starting dosage of Diclegis is two tablets at bedtime. However, “[if] symptoms are not adequately controlled, the dose can be increased to a maximum recommended dose of four tablets daily (one in the morning, one mid-afternoon and two at bedtime).”
An article printed in Medscape from WebMD tracks the history of Diclegis, particularly why it was first pulled from the market 30 years ago and what has changed to allow the drug to hit the market again, which is expected to take place in May.
Diclegis was previously sold in the United States under the brand name Bendectin between 1956 and 1983, but it was pulled from the market because of litigation about birth defects. Although ongoing research has shown that the concerns were unsupported, the drug's previous maker, Merrell Dow Pharmaceuticals, declined to keep making the drug because of the high costs of defending it.
Edward McCabe, MD, medical director for the March of Dimes, told the Associated Press that the birth defect rate was the same among women who used the drug as in those in the general population, creating the false impression that the drug caused the birth defects. "Nothing better has come along" to treat morning sickness in the 30 years since it was taken off the market, Dr. McCabe said. The FDA at the time continued to call the drug safe.
Though Diclegis has been researched, the fact remains that we do not know what effects this drug may have once it hits the general population. Therefore, it should probably be reserved for more severe cases.
Heartbeat recommends that you research and discuss this medication with your medical director, and develop your center’s policy for advising and assisting clients who experience severe morning sickness symptoms.
How involved should medical professionals be?
by Susan Dammann, Medical Specialist

As we stand aghast at the radically pro-abortion Reproductive Health Act recently proposed in New York, we wonder how this could ever happen in our nation. We also have to wonder if this legislation will eventually become a model for laws in other states—or even the nation.
Thankfully, many New York medical professionals have gathered to speak out against the proposed legislation, and they are making their voices heard, striving to turn the hearts and decisions of the lawmakers toward righteous laws.
God has divinely placed many medical professionals within the pregnancy help movement, with unique gifts, callings and expertise that are critically needed in the medical setting. But our influence should not end there. We are also called to inform those who are determining the future of medicine and the lives of our fellow citizens through the laws and legislations that affect medical practice.
We must not be silent in the face of evil, which strives to change the laws of our land, advance the pro-abortion agenda, and eliminate our religious or civil freedom. As Edmund Burke so aptly admonished, “All that is necessary for the triumph of evil is that good men do nothing.”
The honor, respect, integrity, and trust placed in medical professionals must not be wasted, but maximized to create a voice of influence. We have both the right and the duty to be a voice to our local and state community. This is an issue of faith, courage, and principle.
What is at stake? Nothing less than the right to practice medicine according to our conscience and faith. To live in freedom. To save women and children from the devastation of abortion. Even to be free from the coercive power of government.
How are we to implement our precious First Amendment right? As so beautifully exemplified by Dr. John W. Volk in his letter to the editor of the Greeley (Colo.) Tribune, writing articles for publication is one way to get involved.
We can also get involved by participating in local city councils, school boards, testifying during city legislation, introducing pro-life measures to elected officials, and by befriending those in authority and speaking truth to them. Talk radio, op-ed pieces, and more, can also leave a powerful footprint on our world.
Some would ask if we should be vocal in government. Did Jesus call us to sit out the culture war when He said the following?
You are the salt of the earth, but if salt has lost its taste (its quality), how can its saltiness be restored? It is not good for anything any longer but to be thrown out and trodden underfoot by men. You are the light of the world. A city set on a hill cannot be hidden. Nor do men light a lamp and put it under a peck measure, but on a lampstand, and it gives light to all in the house. Let your light so shine before men that they may see your moral excellence and your praiseworthy, noble, and good deeds and recognize and honor and praise and glorify your Father Who is in heaven? (Matthew 5:13-16, Amplified Bible)
Salt acts as a preservative, preventing decay. It is clear that Jesus, in referring to us as salt, is profoundly issuing the command for us to penetrate society, while at the same time keeping evil from penetrating us. Light penetrates darkness. For us to know wisdom and truth, yet hide it is as absurd as lighting a light and hiding it under a basket.
This same mandate is also expressed in Proverbs 1:20-21:
Wisdom cries aloud in the street, she raises her voice in the markets; She cries at the head of the noisy intersections (in the chief gathering places); at the entrance of the city gates she speaks. (Amplified Bible)
Tom Minnery, in his book, Why You Can’t Stay Silent: A Biblical Mandate to Shape Our Culture, brings the biblical truth of Christian citizenship to bear on our everyday lives with the following paragraph:
The proper role for the Christian citizen is to participate in government as fully as his calling and skill can take him, whether it be limited to voting or as an active government leader. When the sparks fly over moral issues in the councils of government, how much more effective it is (and honoring to Christ) to have skilled Christian people at the center of the debate, in full possession of the facts and a record of public trust. Sometimes, of course, this isn’t enough, and the moral position is defeated. But many times the impact of Christian leaders on difficult moral issues has been astounding.1 (Emphasis added)
If we do not speak up and do what we can to influence our culture for righteousness, who will bear responsibility for the results?
As we remember the millions of innocent babies who have lost their lives through abortion, we can take inspiration from the words of Abraham Lincoln in his Gettysburg Address:
It is for us the living, rather, to be dedicated here to the unfinished work … that from these honored dead we take increased devotion to that cause … that we here highly resolve that these dead shall not have died in vain—that this nation, under God, shall have a new birth of freedom—and that government of the people, by the people, for the people, shall not perish from the earth.
Though the challenge may seem daunting and the forces arrayed against us to be great, let us take courage in the fact that after a long hard battle, one president, with the stroke of a pen freed millions of slaves.
This can happen again if we do not ignore our First Amendment rights, and speak out. Whether we are victorious or not, we have been called to be faithful.
Let us take the wisdom, diligence and faithfulness so beautifully displayed within our pregnancy medical clinics and bring it outside the PMC to influence the influential.
Sources
1. Tom Minnery, Why You Can’t Stay Silent: A Biblical Mandate to Shape Our Culture (Carol Stream, IL: Tyndale House, 2002), 58.
Birth Defects: Get Help, Get Connected
Four Helpful Sites
While this is not an exhaustive list, listed below are some references you may want to investigate as possible resources for your center to offer clients with a poor prenatal diagnosis.
- It’s a Mom’s World – Special Needs provides support and information for a mother or couple whose child is diagnosed with special needs.

Samuel Armas -- 21 weeks in utero (FoxNews.com)

Samuel Armas -- 9 years old
(FoxNews.com) - Prenatal Partners for Life is “a group of concerned parents (most of whom have or had a special needs child), medical professionals, legal professionals and clergy whose aim is to support, inform and encourage expectant or new parents. We offer support by connecting parents facing an adverse diagnosis with other parents who have had the same diagnosis. We have many resources such as adoption agencies with clients waiting to adopt and love a special needs child should a parent feel they could not care for them.”
- IsaiahsPromise.net is “a group of parents who knew early in our pregnancies that our babies had severe or fatal birth defects. Each of us, for various reasons, continued the pregnancy. It's a difficult and very personal decision. We know the devastation, confusion, heartbreak and loneliness. We can't change your circumstances or make decisions for you. But we can offer support, friendship and experience.”
- BeNotAfriad.net is “an online outreach to parents who have received a poor or difficult prenatal diagnosis. The family stories, articles, and links within this site are presented as a resource for those who may have been asked to choose between terminating a pregnancy or continuing on despite the diagnosis. The benotafraid.net families faced the same decision and chose not to terminate. By sharing our experiences, we hope to offer encouragement to those who may be afraid to continue on.”
Free Symposium
The First Annual Conference on Medical Advances in Prenatal Diagnoses was hosted by the Council on Poor Prenatal Diagnoses & Therapeutic Intervention in January of 2012.
The conference brought together professionals from many different specialty areas, including genetic researchers, ob-gyn physicians, developmental pediatricians, hospital nursing staff, medical genetic counselors, and medical students. Other participants and guests included peer ministry providers, social service support professionals, advocates for persons with disabilities and public policy specialists.
Julie Armas and her son, Samuel, both spoke at the conference, testifying to the wonderful life Samuel has lived, even with a prenatal diagnosis of spina bifida. The unforgettable 1999 picture of Samuel’s tiny finger reaching out of the womb and grasping his surgeon’s finger was printed in several newspapers worldwide, including USA Today. Samuel turned 13 in December of 2012.
You can view this full-day conference free of charge here.
Prepping for a Healthy Pregnancy
The following information is found at the CDC site:
Not all birth defects can be prevented. But a woman can increase her own chances of having a healthy baby by managing health conditions and adopting healthy behaviors before becoming pregnant. This is important because many birth defects happen very early during pregnancy, sometimes before a woman even knows she is pregnant.
 Here are 10 steps a woman can take to get ready for a healthy pregnancy:
Here are 10 steps a woman can take to get ready for a healthy pregnancy:
- Take 400 micrograms (mcg) of folic acid every day. Folic acid is a B vitamin. If a woman has enough folic acid in her body at least 1 month before and during pregnancy, it can help prevent major birth defects of the baby’s brain and spine.
- Don't drink alcohol at any time during pregnancy. When a woman drinks alcohol, so does her unborn baby. Alcohol in the woman’s blood passes through the placenta to her baby through the umbilical cord. There is no known safe amount of alcohol to drink while pregnant. There also is no safe time during pregnancy to drink and no safe kind of alcohol. Drinking alcohol during pregnancy can cause a baby to be born with a birth defect.
- Don’t smoke. The dangers of smoking during pregnancy include premature birth, certain birth defects (cleft lip or cleft palate), and infant death. Even being around cigarette smoke puts a woman and her unborn baby at risk for problems. Quitting smoking before getting pregnant is best. But for a woman who is already pregnant, quitting as early as possible can still help protect against some health problems for the baby, such as low birth weight. It’s never too late to quit smoking.
- Don’t use “street” drugs. A woman who uses illegal—or “street”—drugs during pregnancy can have a baby who is born premature with low birth weight, or has other health problems, such as birth defects. A woman who uses cocaine while pregnant is more likely to have a baby with birth defects of the arms, legs, urinary system, and heart. Other drugs, such as marijuana and ecstasy, also can cause birth defects among babies.
It also is important that a woman not use "street" drugs after she gives birth, because such drugs can be passed through breast milk to her baby and can affect the baby’s growth and development. If you use "street" drugs, talk with your doctor about quitting before you get pregnant. - Talk to a health care provider about taking any medications. Taking certain medications during pregnancy can cause serious birth defects, but the safety of many medications taken by pregnant women has been difficult to determine. If you are pregnant or planning a pregnancy, you should not stop taking medications you need or begin taking new medications without first talking with your doctor. This includes prescription and over-the-counter medications, as well as dietary or herbal products.
- Prevent infections. Some infections that a woman can get during pregnancy can be harmful to the unborn baby. Learn how to help prevent infections.
- Talk to your doctor about vaccinations (shots). Many vaccinations are safe and recommended during pregnancy, but some are not. Having the right vaccinations at the right time can help keep a woman and her baby healthy.
- Keep diabetes under control. Poor control of diabetes during pregnancy increases the chances for birth defects and other problems for the baby. It can also cause serious complications for the woman. Proper healthcare before and during pregnancy can help prevent birth defects and other poor outcomes.
- Reach and maintain a healthy weight. A woman who is obese (a body mass index of 30 or higher) before pregnancy is at a higher risk for complications during pregnancy. Obesity in the woman also increases the risk of several serious birth defects for the baby. If you are overweight or obese, talk with your doctor about ways to reach a healthy weight before you get pregnant.
- See a health care professional regularly. A woman should be sure to see her doctor when planning a pregnancy and start prenatal care as soon as she thinks that she is pregnant. It is important to see the doctor regularly throughout pregnancy, so a woman should keep all her prenatal care appointments.
 Six tips from the American Pregnancy Association:
Six tips from the American Pregnancy Association:
Awareness and education are the first steps to preventing birth defects. The immediate step following awareness and education is taking action. There are a number of things you can do to increase the probability of having a healthy pregnancy and a healthy baby. Some are more challenging than others because they require that you break habits, but it is worth your effort.
Here are a variety of tips you can use to prevent birth defects as you contemplate starting or adding to your family:
Tip 1. The first and foremost tip is maintaining preconception health; eating well balanced and nutritional meals, and taking a multivitamin daily that includes the recommended 400 mcg of folic acid.
Tip 2. If you are sexually active and pregnancy is a possibility, make sure you take a multivitamin daily which includes the recommended 400 mcg of folic acid and other essential B vitamins.
Tip 3. Avoid all activities that could potentially lead to birth defects including alcohol, tobacco, illicit drugs, and caffeine.
Tip 4. Seek an annual gynecological and wellness exam.
Tip 5. Obtain genetic counseling and birth defect screening, particularly if you have any family history of birth defects or if you are 35 years of age or older.
Tip 6. Help your family or friends who might be considering parenthood by informing them that January is Birth Defects Prevention Month. You can send an e-mail and link to this page to everyone in your address book.”
More recommendations from the CDC:
-
Premature Birth: Important growth and development occur throughout pregnancy – all the way through the final months and weeks. Babies born three or more weeks earlier than their due date have greater risk of serious disability or even death. Learn the warning signs and how to prevent a premature birth.
-
Folic Acid: Folic acid is a B vitamin that can help prevent major birth defects. Take a vitamin with 400 micrograms (mcg) of folic acid every day, before and during pregnancy.
- Smoking during pregnancy is the single most preventable cause of illness and death among mothers and infants. Learn more about the dangers of smoking and find help to quit.
- Alcohol: When you drink alcohol, so does your unborn baby. There is no known safe amount of alcohol to drink while pregnant.
- Vaccinations: Talk to your doctor about vaccinations (shots). Many are safe and recommended during pregnancy, but some are not. Having the right vaccinations at the right time can help keep you and your baby healthy.
- Flu and Pregnancy: If you're pregnant, a flu shot is your best protection against serious illness from the flu. A flu shot can protect pregnant women, their unborn babies, and even their babies after birth.
- Infections: You won’t always know if you have an infection—sometimes you won’t even feel sick. Learn how to help prevent infections that could harm your unborn baby.
- HIV: If you are pregnant or are thinking about becoming pregnant, get a test for HIV as soon as possible and encourage your partner to get tested as well. If you have HIV and you are pregnant, there is a lot you can do to keep yourself healthy and not give HIV to your baby.
- West Nile Virus: Take steps to reduce your risk for West Nile virus and other mosquito-borne infections.
- Diabetes: Poor control of diabetes during pregnancy increases the chance for birth defects and other problems for your baby. It can cause serious complications for you, too.
- High Blood Pressure: Existing high blood pressure can increase your risk of problems during pregnancy.
- Medications: Taking certain medications during pregnancy might cause serious birth defects for your baby. Talk to your doctor or pharmacist about any medications you are taking. These include prescription and over-the-counter medications and dietary or herbal supplements.
- Environmental and Workplace Exposures: Some workplace hazards can affect the health of your unborn baby. Learn how to prevent certain workplace hazards. If you are worried about a specific substance, please click here.
- Unborn Babies Exposed to Radiation: If you think you might have been exposed to radiation, talk with your doctor.
- Pediatric Environmental Health Specialty Units:
A network of experts in children's environmental health.
Birth Defects Fact Sheets
 While there are thousands of different birth defects, the most common are heart defects, cleft lip and cleft palate, Down syndrome and spina bifida. Approximately 150,000 children are born every year in the United States affected by one or more birth defects, according to the American Pregnancy Association.
While there are thousands of different birth defects, the most common are heart defects, cleft lip and cleft palate, Down syndrome and spina bifida. Approximately 150,000 children are born every year in the United States affected by one or more birth defects, according to the American Pregnancy Association.
The CDC reports that one in every 33 babies (about 3 percent) is born with a birth defect, and that birth defects are one of the leading causes of infant deaths, accounting for more than 20 percent of all infant deaths. Causes vary, including the use of alcohol, street drugs, and prescription drugs, being exposed to various infections such as cytomegalovirus or sexually transmitted infections. Genetic conditions can also be passed from parent to child.
Information about Specific Birth Defects
The CDC has great information on many birth defects which you may find useful in your center at the following links:
- Anencephaly
- Cleft Lip / Cleft Palate
- Congenital Heart Defects
- Down Syndrome
- Encephalocele
- Gastroschisis
- Hypospadias
- Omphalocele
- Spina Bifida
- Upper and Lower Limb Reduction Defects
 Cytomegalovirus (CMV) Disease: The Congenital Disease Mothers Don't Know About
Cytomegalovirus (CMV) Disease: The Congenital Disease Mothers Don't Know About
The following information is also found at the CDC site:
CMV is the most common congenital (present at birth) viral infection in the U.S. Each year, about 5,500 (1 in 750) children in this country are born with or develop disabilities that result from congenital CMV infection. More children have disabilities due to this disease than other well-known congenital infections and syndromes, including Down syndrome, fetal alcohol syndrome, spina bifida, and pediatric HIV/AIDS.
CMV is spread from person to person by close contact with body fluids, such as blood, urine, saliva, semen, vaginal fluids, and breast milk. Once CMV is in a person's body, it stays there for life. Most people who become infected with CMV have mild, flu-like symptoms or no symptoms at all; the exceptions are infants with congenital infection or people who have weakened immune systems.
For pregnant women, sexual contact is a common source of CMV infection. Limiting sexual partners and practicing safe sex may reduce the risk of catching CMV.
Another common source of infection for pregnant women is contact with the urine or saliva of young children who are infected with CMV and are shedding the virus.